President's Message

Dr Simon Gabe, BAPEN President
As we approach the end of 2017, I find myself pondering over some data relating to BAPENs core raison d’être and feeling that BAPEN should congratulate itself.
In the summer, we sent out a Freedom of Information (FOI) request to all Trusts/hospitals in the UK in order to find out about the presence and activity of nutrition support teams. When BAPEN was created in 1992, one of the key visions was that hospitals should develop nutrition support teams and nutrition steering committees. BAPEN ran training courses for teams to develop (Grasmere course) and produced standards and guidelines on nutrition support. BAPEN helped to develop the NICE Guidelines on Nutrition Support in Adults (CG32), published in 2006, which recommended that all people who need nutrition support receive coordinated care from a multidisciplinary nutrition support team. So, the question can now be asked: Have BAPENs activities been successful?
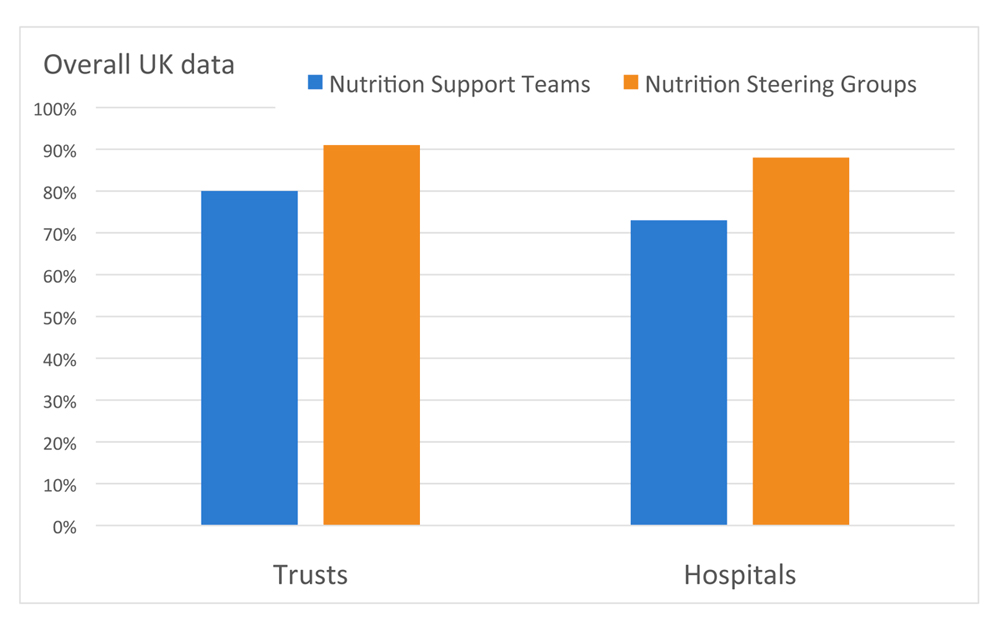
The results of the FOI request will be presented at the BAPEN Conference. At this point of writing we have 67% of returns. It is interesting to see that 80% Trusts and 73% hospitals in the UK now have a nutrition support team (many Trusts have more than one hospital). There are differences between the nations and, in general, England and Scotland are well provided, but Wales and Northern Ireland are not. This is very helpful to see and will help us to focus our attention where it is needed. Almost all Trusts and hospitals had nutrition steering committees, which is a real achievement. More information has been gathered as to the activity and composition of nutrition support teams and also the number of Trusts and hospitals that have business cases in place either for a nutrition support team or for additional members in the teams. Overall, I see this as quite an achievement for BAPEN who has been championing this as a development over the past 25 years.
BAPEN has also championed nutritional screening with the introduction of the ‘Malnutrition Universal Screening Tool’ (‘MUST’). By law every provider organisation is required to make sure the individuals in care have enough to eat and drink to meet their nutrition and hydration needs and receive the support they need to do so. Individuals must have their nutritional needs assessed and food must be provided to meet those needs. BAPEN has developed a web-based Nutritional Care Tool which enables organisations to monitor nutritional screening, the effectiveness of nutritional care they provide and the patient experience.
The annual report will soon be available on the BAPEN website; and 70 organisations are currently registered to use the BAPEN Nutritional Care Tool and all have contributed data at least once since its inception in September 2015. A total of 7,574 patients have been surveyed with this Tool and 37.2% patients were found to be at risk of malnutrition. The majority of organisations are in the NHS acute sector, but there is representation from nursing and residential homes, and community organisations. In addition, 77% of organisations using the BAPEN Nutritional Care Tool reported having a nutrition steering committee and 73% reported having a nutrition support team. This is very similar to the information collected by the FOI request and corroborates these findings.
So where do we go from here? Well, we now need to get the BAPEN Nutritional Care Tool into all care settings not only to help to identify individuals that need nutrition support, but also to enable Trusts to assess how to use their resources appropriately and improve nutritional care for patients. That is what we are here to do. That is a worthy goal. Join us and be part of it.
Return to top