
BAPEN Annual Conference 2020 – Webinar series

BAPEN’s Programmes Committee Members: Pete Turner (Chair) and Jennie Mort (Sovereign Conference), along with Tony Murphy (BPNG), Jo Wakeling (NNNG), David Sawbridge (IrSPEN), Dr Jeremy Nightingale (BIFA), Dr Giles Major (BAPEN Medical) and BAPEN’s Education Officer, Dr Anne Holdoway report on the BAPEN Annual Conference – webinar series.
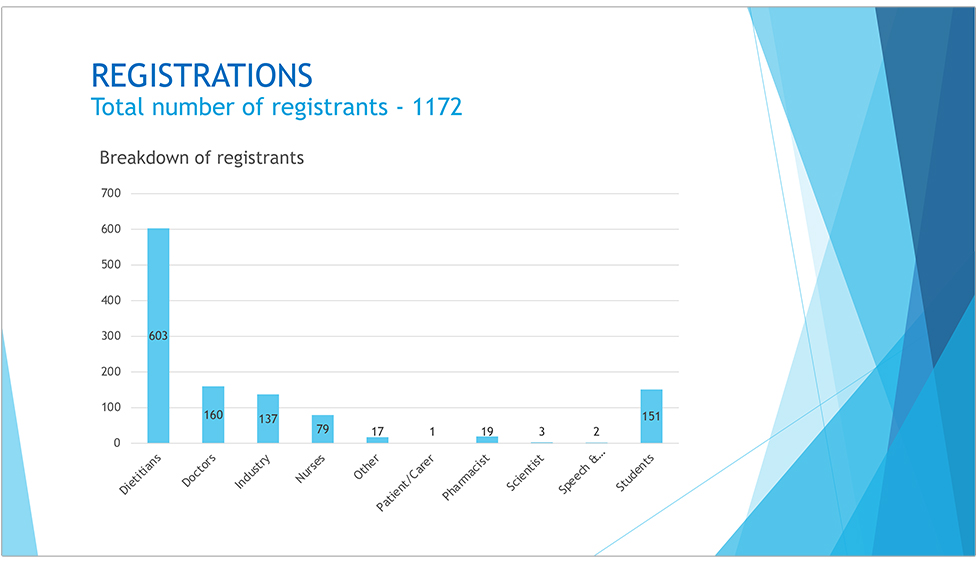
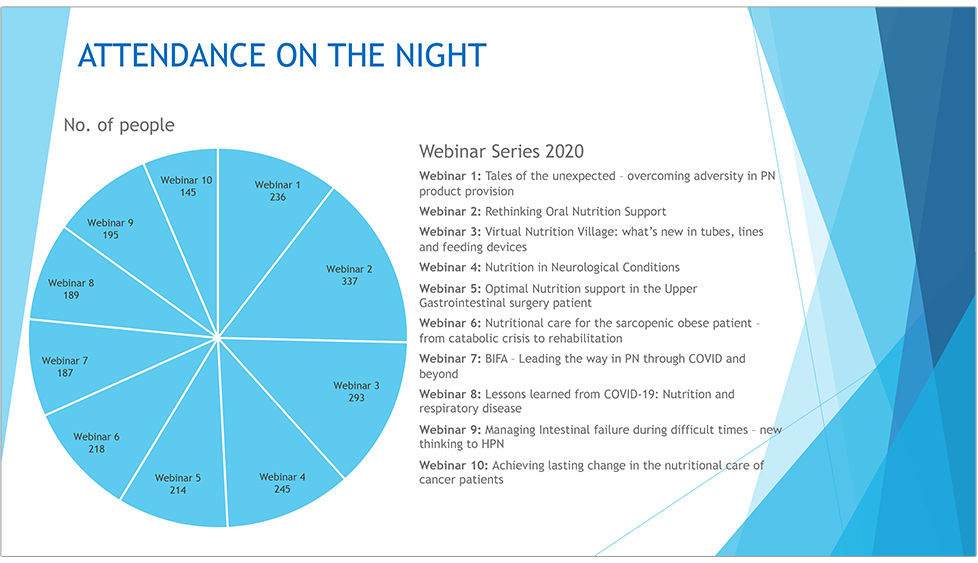
The BAPEN webinar series was a huge success with over 1,100 registrations and evening audiences exceeding 200 delegates on some nights, dialling in from over 14 different countries worldwide.
There is a poignant scene in the opening of the Disney film ‘Bugs Life’ when a big leaf drops on the path of a line of ants. At first there is general panic but before long the ants work out a new path around the leaf. Such a challenge occurred in the provision of home parenteral nutrition (HPN), firstly in the summer of 2019, when there was a sudden shortfall in the commercial capacity to aseptically compound HPN feeds and, secondly, in March 2020, at the outbreak of the COVID pandemic. At the time, all four speakers, who shared presentations in webinar 1, found themselves at the very heart of planning and decision-making to ensure patient supplies of essential nutrition were maintained.

Chaired by Dr Chris Mountford and facilitated by Tony Murphy, webinar 1 started with Carolyn Wheatley, HPN patient and Chair of PINNT, expressing the importance of communication and emphasised the need to ensure patients were given the ‘information they need to know.’ The patient support group PINNT acted as a conduit for patients’ experiences and views into the national network groups that were to form. Carolyn ended her talk with a quote from Benjamin Franklin: “Tell me and I forget. Teach me and I remember. Involve me and I learn.”

Rebecca White, Medical Advisor, Baxter Healthcare Ltd, highlighted how contingency needs to be built into the homecare supply chain from ‘picking’ through ‘dispensing’ and ‘delivery’. The UK model is heavily reliant on aseptic compounding of ‘tailored’ HPN, which is particularly vulnerable to adversity, requiring highly trained staff, cold chain transport, and with an expiry of just two weeks it is not possible to prepare contingency stock. However, out of adversity, came positive initiatives; the setting up of new channels of communication between industry partners, homecare companies, and the NHS; and an openness to new models of service provision. The use of multichamber bags (MCBs) in combination with intravenous fluids played a significant role in contingency planning. Whilst not nutritionally complete (for lack of vitamins and trace elements) the use of MCBs will need to be considered as part of ‘blended approaches’ to HPN provision.

Dr Trevor Smith, Consultant Gastroenterologist, University Hospital Southampton, presented a clinical and national perspective. Trevor chaired the NHS England HPN Clinical Support Cell. This multidisciplinary group was set up in July 2019 and has met twice a week since. The group developed a system for clinically prioritising those patients most at risk, including: children, patients with advanced malignancy and poor prognosis, ultra-short bowel, high volume outputs, and pregnancy. 740 applications for HPN support have been reviewed, and recommendations have been made for contingency planning for those patients who would require tailored aseptically compounded HPN (high risk), those patients who could be managed with MCBs and additional IV fluids for 2 weeks (medium risk), and those who could be managed similarly for 4 weeks (lower risk). A survey of all UK intestinal failure (IF) units was made, and nationwide contingency arrangements set up for the emergency admission of IF patients. BAPEN’s COVID-19 resources and BIFA’s Top Tips papers and position statements proved invaluable for decision making.

Uche Meade, Pharmacy Manager, St Mark's Hospital, Harrow, gave the final presentation and this was a fitting tribute to the hospital staff at St Mark’s, mirroring the huge effort and professionalism of nutrition teams country-wide. With over 300 patients on HPN, the task that faced St Mark’s was considerable. A trust-wide approach was needed and included fast decisions on: finance and purchasing, the setting up of special out-patient clinics for patients on MCBs with on the day rapid biochemistry testing, and the development of an online tool to record, assess and track calculated nutritional requirements vs actual nutrition prescribed. Initially, requests were made to GPs for the supply of oral trace element and vitamin supplements, but later this service was transferred to the homecare companies. It was the detail that was so impressive - for example, making sure patient records for contact numbers and email addresses were up-to-date, arranging refresher training on person-centred care for the team, sending patients online links to videos. At the end of her talk Uche put up a slide with two photos of all the staff who had contributed to making sure patients received ‘safe’ nutrition support during difficult times. Her final words sum it up: “We put patients at the heart of everything we did.”
Much has been learnt during the past months, and valuable networks set up that continue to build resilience into the provision of nutrition support. In his presentation, Trevor advised to “remain agile to solve problems” – and that is poignant.
Over the years there has been considerable debate on the effectiveness of oral nutrition support. With a new global initiative on malnutrition, this webinar sought the opportunity through a panel of experts to take stock and rethink strategies on optimal oral nutrition support in the community. Chaired by Linda Cantwell and Carole-Anne Fleming and facilitated by Dr Anne Holdoway, three expert speakers reflected on treatment strategies, the importance of accounting for system-wide cost pressures, the creation and funding of pathways of care and what is best for patients.

Shailen Rao, Managing Director, Soar Beyond, started the session and sought to inspire listeners to consider how integrated care systems can be used as a pivotal force to support business cases for identifying and providing first line treatment for malnutrition. Drawing on his experiences as a pharmacist and former head of medicines management, Shailen put into context the cost of failing to act and the importance of determining costs across the system and the drawbacks of cost cutting exercises focused on cutting nutrition support products. Shailen demonstrated how proactive management of malnutrition in the community through leadership, training and education to empower non-experts in nutrition with escalation for more complex cases can be both clinical and cost effective. Shailen urged those working in this field to encourage moves to prioritise actions in a systematic way and how the advent of Primary Care Networks (PCNs) provide a springboard to call for the additional capacity necessary to enable proactive identification and management of people who are at risk of malnutrition. Shailen emphasised how dietitians were the natural system leaders, ideally placed and skilled to collaborate with other members of the primary care team to lead on initiatives to raise awareness of how good nutrition could improve care within local health systems.

Following on from Shailen, Emily Walters, Dietitian & Clinical Researcher, University of Southampton, explored ‘Beyond screening – how malnutrition sub-types guide treatment’. With extensive experience as a clinical dietitian and a researcher and leader in the field of malnutrition, Emily provided a succinct and eloquent overview of malnutrition, the purpose of screening tools to identify risk and the importance of undertaking a comprehensive, holistic nutrition assessment in those at risk to determine appropriate interventions that are likely to achieve success. Emily touched upon the importance of differentiating the sub-types of malnutrition, the need to establish if the malnutrition is social or disease-related or a combination, and if disease was present explained how inflammation and disease processes can influence the effectiveness of interventions. Utilising the evidence-base and describing its limitations, Emily provided key insights into the likely success and appropriateness of interventions and emphasised the importance of anticipating the impact of disease and inflammation on appetite and the ability to take adequate oral nutrition. Emily’s questioning style of delivery, and exploration of the evidence-base, stimulated the question as to why the evidence-base for treating disease-related malnutrition frequently demonstrates the value of medical nutrition combined with dietary modification, whereas in contrast malnutrition resulting from social or economic problems might respond to food-based and supportive interventions. Emily utilised a case study to illustrate how careful history taking, nutrition assessment to identify the underlying factors that can contribute to the evolution of malnutrition, guide clinical decision making to help determine appropriate nutritional care.

The final presentation in the webinar, ‘Embedding nutrition services into primary care – insights and opportunities’ was delivered by Tanya Rumney RD, Lead Therapist for Nutrition and Dietetic Service, Primary Care AHP Ambassador for Health Education England, Cheshire West Integrated Care Partnership. As a Lead Therapist for Nutrition and Dietetics, Tanya shared key insights into the service innovation she led on to drive forward the development of services to manage malnutrition in primary care, including preventative strategies. Building on Emily’s presentation, Tanya further highlighted the complexity of malnutrition, both its development and management. With such considerable numbers at risk and many receiving a late diagnosis of malnutrition and a missed opportunity to intervene earlier, Tanya emphasised the role of dietitians in influencing and empowering the wider workforce in primary care to tackle malnutrition in a timely manner and reverse and realise the cost savings in taking early and preventative action – for example, through training and education in care homes and amongst community providers. Echoing Shailen’s key message, Tanya concluded with a call to action describing how Primary Care Networks present the dietetic profession with key opportunities to lead on promoting the delivery of optimal nutritional care, care that goes beyond treating malnutrition but addresses the overall holistic needs of clients taking into account the presence of a range of clinical conditions, co-morbidities and patients self-determined goals. A lively discussion followed with numerous questions and answers from one of the largest audiences of the webinar series.
On 11th November 2020, BAPEN hosted the third in a series of Webinars, bringing together expert speakers on three diverse but related topics for the Nutrition Village, thanks to its success at conference in Belfast last year.

First up was Angela Cole, Clinical Nurse Specialist for Children with Intestinal Failure at Royal London, whose topic was ‘The Triangle of Transition and Independence’. Tying her presentation to the case of a young man under her department’s care in her early years in practice, she recounted elements of his journey from childhood to a place at university a long way from home, highlighting some of the issues and concerns he faced. Much effort has been invested over the years to facilitate a smooth transition for young people with intestinal failure – from the care of their parents/domestic carers and the paediatric services to a life of independence as a young adult. As a result, outcomes are now routinely much improved, as teams have learned to deal with not only the clinical needs of the young person, but emotional, social, educational, and vocational requirements too. Tools deployed include bringing the paediatric and adult teams together, to present a coherent face to the young person and their parents/carers, and doing so at an early stage through regular clinics, allowing each party to familiarise itself with the others in a triangle of care. Further literature and support for this topic can be found through PINNT.

'Life Lines – Innovations in practice improving and enhancing the patient's journey’ was the second topic introduced by Shakeel Herwitker, Pharmacist, Liverpool University Hospitals NHS Foundation Trust, and expanded upon by his colleague, Alison Young, Consultant Nurse in Nutrition, Royal Liverpool and Broadgreen University Hospitals NHS Trust. The 2013 launch of the construction of the ‘New Royal Hospital’ in Liverpool gave the Trust the opportunity to integrate its Home Parenteral Service, complete with a manufacturing facility and sophisticated software, to ensure that the correct preparation of PN was formulated, documented, and delivered to each patient. At the ‘sharp end’ of this process is the placement of an appropriate central venous access device (CVAD) in a patient, and Alison’s presentation outlined some of the available equipment options in different situations. Placement itself is critical, and whereas ultrasound represented a step forward in locating blood vessels, the Sherlock 3CG system now allows the progress of the tip to be monitored towards its final site within the body and adjusted if necessary before treatment commences. Alison also introduced the ambulatory.

Expanding on the subject of ‘line placement’, Dr Trevor Smith, BAPEN President, introduced a presentation by Wendy Hurst, Senior Product Manager EMEA, Digestive Health, Avanos, on ‘Getting It Right First Time’, concentrating on the placement of nasogastric feeding tubes. Accidental delivery of nutrients of medicines into the respiratory tract is a potentially fatal ‘Never Event’, so it is imperative that staff fitting nasogastric (NG) tubes get it right – and it must be remembered that in the current pandemic some of these nurses have been away from the NHS or have worked in different specialisms. The Avanos ‘Nasogastric app’, for both Android and Apple smartphones, provides a straightforward aide-memoire to the procedure, including essential tips as it steps the nurse through the procedure, as well as linking to other resources for further information. While in no way a replacement for training, it helps reinforce what has been learned, sequentially addressing placement, confirmation, and questions to ensure placement is correct and to identify knowledge gaps. This app is supported by the NNNG, BAPEN and the current NHS improvement service. Developed for clinicians by clinicians. Download the App today! Search NG tube and the Avanos icon.
Several themes emerged across the speakers’ contributions, however. Whilst standardisation is key, in minimising human error and increasing safety, each patient remains a unique individual, and must be treated as such, even – in some difficult cases – if other conditions prevent them from achieving full independence. The current COVID-19 pandemic has impacted the delivery of enteral and parenteral nutrition in many ways, from the conversion of many clinics from ‘face-to-face’ to virtual, the difficulty in obtaining bespoke feed bags (and therefore the necessity of topping up with vitamins via a second pump or dual pump system), complications in the needs of COVID patients requiring nutrition to be given, and in the ‘ground-glass’ X-rays obscuring views of the PICC line tip location, and the influx of nursing staff to the discipline.
COVID-19 resources are available from the BAPEN website and are constantly updated. A search for ‘NG tube’ will find the Avanos app referred to, and this is live and available now. Over the course of 80 minutes or so (including a Q&A session), an interesting series of presentations was well received. The webinar was chaired by Dr Andrew Rochford and facilitated by Jo Wakeling, but would not have been possible without Avanos and BD, the technical team and those behind the scenes ensuring the glitch-free video link, ………………………. oh and the Amazon delivery man!
With many patients with neurological conditions at risk of malnutrition as a result of a deteriorating swallow and reduced ability to eat and drink, this webinar examined thinking beyond nutrients. Chaired by BAPEN’s president Dr Trevor Smith, and facilitated by Dr Anne Holdoway, this webinar explored how practitioners might ensure that decisions on nutrition support remain centred on the patient, how we might mitigate for risk when oral feeding becomes difficult and how nutrition is integral to function and quality of life.

Professor Chris McDermott’s passion as a Consultant Neurologist to further develop the evidence base for delivering supportive and symptomatic care for patients living with motor neurone disease (MND), including nutrition, was evident in his opening presentation. Professor McDermott described how he was struck at an early stage in his career as a neurologist by the terrible suffering facing those living with MND/amyotrophic lateral sclerosis (ALS), which led to the motivation to not only to be part of the effort to understand the pathogenesis and trial new treatments but to ensure that care delivered to people living with MND is evidence-based. Professor McDermott introduced the audience to the trials currently underway in Sheffield to improve the nutritional care of patients with MND, including the OptiCALS study; a new multi-centre trial which aims to investigate the benefits of a high calorie diet in MND.

Professor McDermott’s presentation was followed by an inspirational presentation from Sean White, an experienced Home Enteral Feed Dietitian and co-researcher on the NIHR programme grant, HighCALS, led by Professor McDermott, and which is focused on how to meet the nutritional needs of people with MND. Sean’s experience in nutrition support was evident in his presentation that stimulated the audience to consider how we might provide effective nutritional care for people affected by MND, including timeliness of discussions and detailed explanations that are required to enable patients to undertake the complex decision as to whether to have a gastrostomy placed or not. As Home Enteral Feeding Lead for PENG and with many years’ experience in supporting patients on home enteral tube feeding, Sean shared insights on the role of vigilance and monitoring by all members of the multidisciplinary team (MDT) and the importance of on-going dietetic input for those on home feeding once the tube has been placed. Sean provided a convincing argument for care pathways to integrate essential systematic frequent monitoring of people with MND, incorporating a low threshold for escalation of nutritional intervention to prevent irreversible deterioration in nutritional status, function and well-being.

For many of us working with patients with swallowing difficulties we will be aware of patients who desire to continue with oral feeding even when swallowing is deemed unsafe. Building on the nutritional challenges in MND presented by Professor McDermott and Sean, Katie Harp, Clinical Lead Speech and Language Therapist, the Royal Hospital for Neuro-disability in Putney, outlined the issues we face as professionals when supporting patients who might wish to continue to take nutrition and fluids orally in the presence of known risks. With this topic being an area of key consideration and debate within the speech and language therapy profession and in the, shortly to be published, update of the Royal College of Physicians ‘Oral feeding dilemmas’ guide, Katie provided an update on the use of terminology in this area and why guidance is required. Using a case study, Katie outlined the key factors to consider when supporting an individual through what can be a challenging decision-making process for both professionals, patients and carers alike.
The subsequent question and answer session demonstrated the hunger amongst the audience for further research in this field and the limitations of applying population norms – for example, in determining the ideal body mass index and energy requirements to the population with MND.
Surgery involving the upper gastrointestinal (GI) tract may be associated with significant nutritional complications, not encountered elsewhere in peri-operative nutritional support. This multidisciplinary webinar, chaired by Sarah-Jane Hughes and facilitated by David Sawbridge, took us on a fascinating trip through the surgical challenges, perioperative nutritional support and hormonal background to upper GI surgery.
Our three experts provided a variety of clinically relevant and scientifically supported take-home points.

The Mechanisms of Unintentional Weight Loss after Oesophagectomy
Prof Carel le Roux, Co-Director Metabolic Medicine Group, University College Dublin

Feast and Famine – The nutritional landscape of UGI surgery
Kellie Owen, Trainee Advanced Clinical Practitioner, Salford Royal Foundation Trust

Oesophageal Cancer: A surgeon’s perspective
Prof John Reynolds, Professor of Clinical Surgery, St James's Hospital and Trinity College Dublin
- Beware unintentional weight loss after oesophagectomy. Hormonal adaptations lead to an increased sense of satiety and decreased appetite due to gut adaptation. This can be mitigated to some extent by decreasing levels of gut satiety hormones, such as PYY and GLP-1, for example, through the use of somatostatin analogues, in the long run to improve quality of life and post-operative recovery.
- Peri-operative dietetic management requires a multi-disciplinary approach with a focus upon prehabilitation, micronutrient management and a planned post-operative feeding approach. Early nasojejunal tube feeding can help guarantee post-operative nutritional intake and speed recovery, compared to oral feeding alone.
- Again, peri-operative nutritional assessment and management is key to improving outcomes, especially in the upper GI cancer patient, who is already at significant risk of malnutrition. Close nutritional follow-up and supplemental calories may well be required to mitigate a degree of anticipated weight loss.
This webinar emphasised the importance of close nutritional monitoring and forward-planning, together with the difficulties a patient may face in peri-operative upper GI surgical setting.
With COVID-19 shining a light on some of the challenges in providing nutritional support to obese and overweight patients this webinar, chaired by Dr Ann Ashworth and facilitated by Dr Anne Holdoway, sought to take a wider view on the challenges faced by practitioners in determining energy and protein requirements in overweight and obese patients requiring nutrition support.

With an extensive background in clinical practice in critical care and nutrition support and as a key player in the group of authors who updated the PENG Pocket Guide to Clinical Nutrition requirements section, Dr Clare Soulsby presented an insightful and thought-provoking presentation on estimating energy and protein requirements in obesity.
With knowledge gained from her clinical and research career, and the considerable work and efforts in being part of the team undertaking the systematic review of energy requirements and a systematic review of published guidelines on protein requirements, Clare brought to life for the audience, the challenges in determining energy and protein requirements for overweight and obese patients. Utilising her advanced interpretive skills, Clare demonstrated the limitations of the existing evidence base, primarily due to the few studies that have measured energy and protein requirements in obese patients requiring nutritional support. With the paucity of evidence, Clare stressed the need to view the recommendations as ‘expert opinion’ when utilising them for clinical decision-making and emphasised the key role of monitoring of obese patients in receipt of nutritional support, urging all to utilise techniques available locally to assess changes in lean body mass to guide decisions, until such time as further evidence is available and state of the art techniques of assessment are available for all.

Richard Kirwan, Post-graduate Researcher, Department of Biological and Environmental Sciences, Liverpool John Moore’s University, built on Clare’s presentation sharing insights from his research on the importance of muscle mass in cardiometabolic health and provided a thought-provoking session on how to maintain muscle in ‘at risk’ populations, including those affected by COVID-19. With an introduction covering the extent and rapid nature of muscle loss arising during extended hospitalisation, Richard prompted the audience to consider its consequences for long-term health and body composition especially in patients with obesity. Mechanisms of muscle loss, long-term health effects, the impact of muscle wasting on appetite and sarcopenic obesity created the foundation to then explore countermeasures, utilising dietary modifications (protein dosing and timing) and exercise interventions to increase lean mass and reduce cardiometabolic risk as currently being investigated in cardiac rehab populations who share commonalities with COVID-19 patients.
The questions and answers considered early indications that patients who have experienced a severe infection of COVID-19, and lost significant amounts of weight during the catabolic storm associated with COVID-19, regain weight after discharge but that a disproportionate amount may be fat mass relevant to muscle as a result of fatigue and breathlessness, resulting in low levels of activity and sedentary behaviour combined with comfort eating. The importance of utilising knowledge and strategies to reduce muscle loss through dietary and exercise interventions to increase lean mass that have been developed in cardiac rehab populations, may indeed shed light on the rehabilitation needs of those surviving a severe case of COVID-19, many of whom were overweight or obese with poor cardiovascular health.
Ultimately, the webinar highlighted the need to enhance our understanding on nutritional requirements in acute illness amongst acutely unwell overweight and obese populations and represents a fruitful area for further research. In the meantime, lessons learned from non-COVID patient research, provides insights into how we might better manage and support the thousands of patients affected by and recovering from a severe episode of COVID-19.
This webinar, chaired by Sarah Zeraschi and Dr Michael Glynn and facilitated by Dr Jeremy Nightingale, aimed to highlight two BIFA Top Tips articles and a recently undated position statement (see references below).

The first talk entitled ‘Nutritional/fluid support in critical care patients with COVID-19’ was delivered by Dr Nicky Wyer, Senior Specialist Dietitian, University Hospital Coventry & Warwickshire. The COVID-19 pandemic brought new challenges to the trust and a significant increase in critical care beds. During this time, Dr Wyer’s role changed to address these challenges and she clinically led, developed, organised and supported a team of dietitians to provide care to those patients requiring critical care. Dr Wyer shared her experiences of primary and secondary COVID infections and emphasised that COVID patients have high energy requirements. Often it is not recognised when enteral feeding is failing to meet these high requirements and it is then that parenteral nutrition should be given. Parenteral nutrition (in a low volume) may be more commonly used in critical care during this second wave of COVID.

This was followed by a case presentation of two patients going home/to a hospice on palliative parenteral support during the first wave of COVID-19 and was presented by Dr Mani Naghibi, Gastroenterology and Human Nutrition Consultant and Nicola Vernon, Dietitian at St Mark’s Hospital, Harrow. They discussed 24-hour infusions, optimising the enteral route of feeding (often low fibre), and using multi-chamber bags (MCBs).

Finally, Antje Teubner, Assistant Specialist in Intestinal Failure at Salford Royal NHS Foundation Trust, gave a summary based on BIFA documents and her unit’s experience about sending patients with advanced malignancy home before, during and after the pandemic. The emphasis was on MDT discussions, having clear aims and plans of when to stop, the use of MCBs, telemedicine and remote discharge.
There was a long discussion with many submitted questions which inevitably overran and included questions about cost/ethics and monitoring.
BIFA publications referenced:
- Jeremy Nightingale, Rebecca White, Nicky Wyer, Richard Leach and the British Intestinal Failure Alliance (BIFA) Committee. Top Tips for the Use of Parenteral Nutrition in Critically Sick Patients with COVID-19.
- Lucy Eldridge, Kirstine Farrer, Loraine Gillespie, Jessica Bower and Clare Shaw. Top Tips for the Oral/enteral Nutrition and Home Parenteral Support for Patients with Small Bowel Obstruction due to Advanced Malignancy during the COVID-19 Pandemic.
- Mani Naghibi, Jeremy Woodward, Penny Neild and the BIFA Committee. The British Intestinal Failure Alliance (BIFA) Position Statement: Palliative parenteral nutrition (HPN) for patients with malignancy.
With COVID-19 presenting an array of new challenges for healthcare teams, this webinar, chaired by Dr Barry Jones and facilitated by Dr Anne Holdoway, reflected on our learnings to date in providing nutrition support in patients with severe COVID-19 infections in intensive care and beyond.

Dr Judith Merriweather, Critical Care Dietitian/Critical Care Recovery Lead/NRS Clinician, Royal Infirmary of Edinburgh, provided a comprehensive overview of the clinical consequences of COVID-19, patient-related factors and ICU treatments that interact to influence the provision of nutritional support in ICU and its success. Drawing on her involvement with many patients in the clinical setting, her own research in the RECOVER study (a randomised clinical trial that looked at the effect of providing increased hospital-based physical rehabilitation and information provision and information needs amongst ICU survivors), her role as Critical Care Recovery Service Lead in NHS Lothian and the active forum of the BDA critical care dietitians group, Judith shared a feast of skills and experiences with the audience. The multiple challenges overcome in the intensive care setting illustrated the rapid knowledge gained in the first surge of the pandemic and amongst the breadth of data shared Judith’s key messages highlighted the importance of continuing with tailored nutritional support during the recovery phase of critical illness in order to promote physical and functional recovery closer to the patient’s pre-COVID state of health.

With a high-profile role within BAPEN as Chair of Programmes and a wealth of experience in critical care nutrition, the nutritional management of intestinal failure and a leading author in creating the BDA/BAPEN response on the route of nutrition support in patients requiring non-invasive ventilation (NIV) or continuous positive airways pressure (CPAP) during the COVID-19 pandemic, Pete Turner, Nutrition Support Dietitian, Ulster Hospital, presented on how we might use COVID-19 as a springboard for change in managing respiratory nutrition. Providing continuity from last year’s conference symposium on chronic obstructive pulmonary disease (COPD), Pete described the barriers to successful oral feeding in acutely unwell patients with respiratory disease, including those with COVID-19 and the rationale and reasoning to potentially explain the resistance to tube feeding patients on NIV and CPAP. With practical insights into the devices available, how to overcome the challenges faced at ward level to successfully tube feed patients on NIV and CPAP, Pete galvanised our attention to the potential solutions for the successful provision of tube feeding, facilitating our understanding of nutrition support for those on non-invasive forms of ventilation and debunking myths underpinning a reticence to provide enteral nutrion support in this group of patients.

With nutrition in intensive care being spotlighted in the pandemic across a range of clinicians, Dr Shameer Mehta, Consultant Gastroenterologist, University College London Hospital, reminded the audience of the resemblance between the causation, metabolism and physiological features of COPD and COVID-19. Shameer highlighted pertinent themes on managing undernutrition in COPD applicable to the COVID-19 cohort including the value of embedding screening into everyday practice, identifying sarcopenia where possible, using digital technology to assess and communicate remotely and provide clear nutritional plans upon discharge. Shameer emphasised the collaboration COVID-19 had provided and presented the opportunity to change minds and galvanise knowledge and actions to ensure patients adversely affected by COVID-19 could benefit from an integrated approach to nutrition across cross settings with access to good quality information.
The three presentations and valuable insights gained through the questions and answer session, demonstrated the immense gains achieved through the efforts of many, the removal of professional and geographical boundaries to enable collaboration and multidisciplinary actions at a local, national and international level, that contributed to the provision of safe and effective enteral nutrition support in hospitals managing the surge early on in the pandemic. Top tips for providing enteral tube feeding to those on NIV and CPAP, understanding and accounting for the global differences in methods of nutritional support (enteral and parenteral nutrition) and how we might use the COVID-19 as a springboard to improve nutritional care amongst those with respiratory disease featured throughout this first-class webinar.
There have been some major challenges in the management of intestinal failure in recent times from shortages of parenteral nutrition (PN) products to the COVID-19 pandemic. Webinar 9, chaired by Sarah Zeraschi and facilitated by Dr Giles Major, took a fresh look at how we support people with intestinal failure to have the best possible quality of life.

Professor Alastair Forbes, visiting Professor, University of Tartu in Estonia, took us through the assessment of quality of life of people using home parenteral nutrition (HPN), paying tribute to decades of work driven by Dr Janet Baxter. This has led to the validation of the HPN-QoL® questionnaire. A key take home message was that quality of life (QoL) on HPN is similar to that of patients on haemodialysis: a useful comparison to express the burden they face. Many factors affect QoL so the tool may be most useful to track change in one person’s experience, although comparisons between people and groups will be possible with large data sets. The discussion reflected on whether widespread adoption would allow standardised assessment across HPN centres, and the increasing importance of measuring quality of life to assess the impact of any new interventions.

Two colleagues, Arun Abraham and Maria Barrett, both from Salford Intestinal Failure, then gave a fantastic tandem talk, taking opposing sides to debate whether ‘Every HPN user’s quality of life would be better with a compounded bag’. Maria (for) emphasised the importance of matching nutritional input to patient’s specific requirements, and the importance of accounting for less obvious factors, such as micronutrients. Arun (against) highlighted that satisfaction is influenced by expectations, and that the care team’s presentation and biases in how PN support is provided will affect a patient’s perception of the care package they receive. Many other countries use less individually compounded PN than the UK. They both agreed that patients need a tailored nutrition care plan and the products used to provide that plan should be a secondary consideration, not the primary aim.

Last, but not least, Dr Siddartha Oke, Consultant Gastroenterologist and Clinical Lead for Nutrition at The Hillingdon Hospitals NHS Foundation Trust, gave a superbly comprehensive overview of the current evidence for the use of hormonal therapies to improve gut function and reduce reliance on PN. Clinical response varies by patient; and although data on larger groups of patients is needed, response does seem to associate with improvements in quality of life. New products are in development and it is hoped that this will reduce patient burden and provider costs so that more patients can benefit from effective therapy.
With the pandemic disrupting cancer services, this webinar explored the importance of timely diagnosis in the oncology patient, the role of nutrition across the continuum of care and how the staging of cancer is linked to nutritional status, cachexia, malnutrition and sarcopenia. Chaired by Dr Andrew Rochford and facilitated by Dr Anne Holdoway the webinar sought to uncover how we might improve the nutritional care of cancer patients during treatment and beyond.

With a specific interest in the value of nutrition in oncology, Professor Robert Thomas, Consultant Oncologist, Bedford & Addenbrooke's Cambridge University Trusts, described how nutritional issues feature strongly in most routine consultations. He described the information and answers patients and carers sought and our current knowledge and future needs to create a greater understanding of the role of nutrition and specific nutrients on outcomes and effectiveness of oncology treatments, including the new immune modulating targeted therapies. How to avoid weight gain or loss and supporting patients towards the end of adjuvant therapies or patients with metastatic disease, Professor Thomas also highlighted the strong desire to understand how nutrition might facilitate long-term control of disease, reduce the risk of relapse and optimise health using diets that mitigate the increased risk of chronic degenerative diseases after cancer, including arthritis, osteoporosis, hormonal changes and heart disease. Looking forward, Professor Thomas also touched on the role of gut health, oxidative stress, chronic inflammation, immunity and epigenetics and how nutritional issues are directing current and future studies on the use of specific supplements, probiotics and a range of dietary and lifestyle measures.

Drawing strongly on her doctoral studies, Erin Sullivan, Research Dietitian, Clinical Nutrition Research Group, University College Cork, provided a breath-taking tour of current understandings of cachexia and sarcopenia, including how we might seek to assess this in practice. Erin deftly presented key data summarising the abnormalities in body composition that are highly prevalent in cancer, at all ranges of body mass index (BMI), and how such changes are associated with poor clinical and patient-focused outcomes but are commonly missed if we are to rely on simple screening. Erin stressed the imperative rationale to identify patients who may be experiencing changes in body composition without reaching a typical cachectic appearance. With frequent weighing for dosing of systemic treatments, and opportunistic availability of CT or MRI scans to identify muscle and fat changes, Erin highlighted how even in current practice, routine nutritional screening and detailed nutritional assessment is feasible and yet despite this, the readily available information is not being used. To improve nutritional care and work towards efficacious interventions for malnutrition and cachexia in cancer, Erin urged those involved to work towards a goal to ensure that trends in weight are noted and acted upon promptly, not just in terms of modifying chemotherapy dose but also initiating a referral to dietetics for full nutritional assessment and management at an early stage in the disease course, where dietetic intervention has potential to improve outcomes.
Delivering the final presentation in the entire series of webinars, Mhairi Donald, Macmillan Consultant Dietitian, Brighton & Sussex University Hospitals NHS Trust, provided personal insights into the combined effects of the COVID-19 pandemic and cancer on patients in her presentation entitled ‘Caught between the 2 big C's – Cancer and COVID’. As a Consultant Dietitian at the Sussex Cancer Centre for the last 12 years, supporting people affected by cancer through the course of their journey from diagnosis and treatment through to survivorship and palliative care, Mhairi articulated the impact of cancer, its treatment and side effects on food intake, pleasure, routines and the daily rhythm of life. Emphasising the need for comprehensive and holistic assessments, Mhairi demonstrated how skilled practitioners can support patients and families to overcome challenges relating to eating and nutrition which offers the capacity to enhance the quality of life for patients and family members and transform the patient experience. Highlighting the broad range of physical, emotional and social issues experienced by people affected by cancer and exacerbated by the conditions created during the COVID-19 pandemic relating to delayed treatments, shielding, difficulties shopping and isolation, Mhairi demonstrated how services were adapted, how innovations took place at pace, and how the detailed assessments and good quality resources enabled dietetic services to continue to offer tailored advice that was holistic in nature, individualised and truly patient centric.
The question and answer session sought answers from the panel on how we might encourage oncologists nationwide to: recognise the role of dietary counselling; gain support to fund dietitians in oncology; further develop nutrition assessment tools in practice; test the role of novel nutrients in the future; and ensure that nutrition is an integral component of the entire cancer journey from diagnosis, pre-treatment, during treatment and post-treatment, including long-term health in the increasing numbers of patients living with and beyond cancer. Time ran out to discuss the role of oral nutritional supplements in cancer but, as suggested by Andrew Chairing the session, there lies within an entire topic for a future symposium at our next conference.
With thanks…
Each webinar was supported by an unrestricted education grant from our industry colleagues and we again thank them for supporting these webinars.

Virtual webinar series available on demand
If you missed the chance to view any of the webinars, you can access all the webinars including the BAPEN Medical day on demand at a time convenient to you. Remember as a BAPEN member, access to all is completely free! To access: click here.

