News Round-up
Malnutrition pathway launches new fact sheet to advise on dealing with patients with sarcopenia
In light of the increasing evidence on the importance of preserving muscle mass as we age1, the Malnutrition Pathway (www.malnutritionpathway.co.uk) has developed a new fact sheet focusing on sarcopenia.
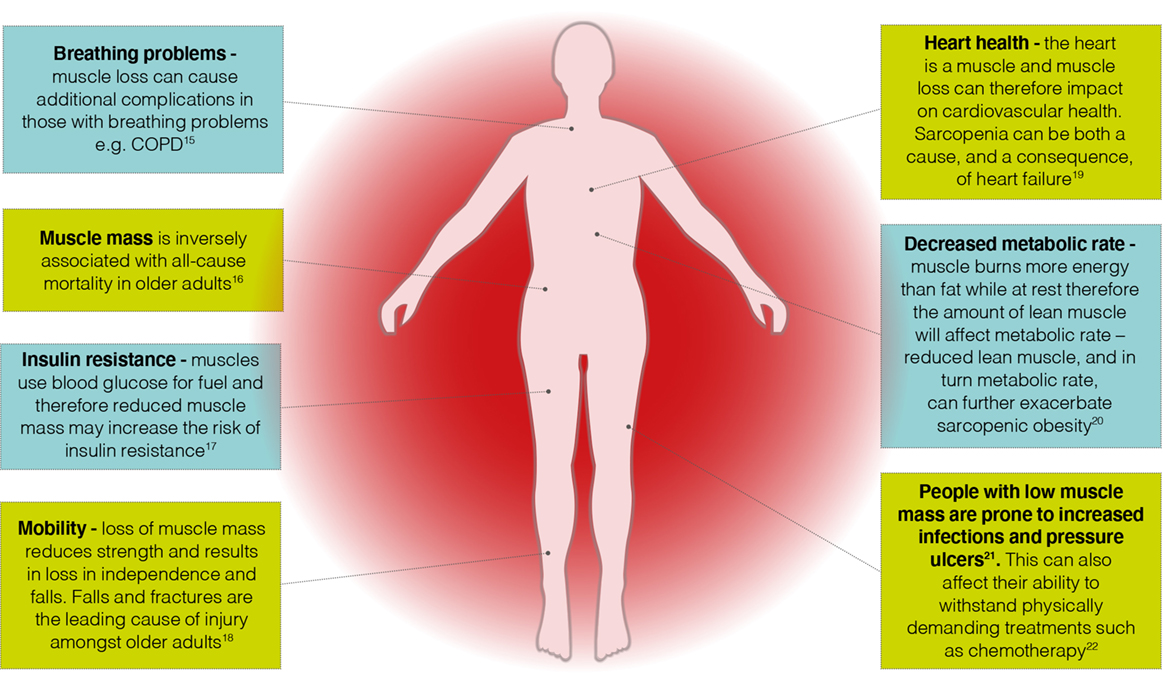
Disease, inactivity and poor nutrition can all contribute to sarcopenia and while it is more common in older age it can also occur in earlier life2. If left untreated, sarcopenia can affect recovery from surgery or injury3, hamper response to treatment4, reduce functional capacity5, 6 or contribute to a more rapid deterioration in pre-existing conditions5, 6, 7 (see Figure 1).
Written by consultant dietitians, Dr Ann Ashworth and Dr Anne Holdoway, the new sarcopenia fact sheet outlines why it is important to identify sarcopenia in all patients whether they are underweight, normal weight, overweight or obese. It summarises the multiple factors that can contribute to sarcopenia and the potential consequences to health, giving practical advice on diagnosis and treatment according to the patient’s current nutritional status. The fact sheet gives advice on how to identify sarcopenia and malnutrition, detailing the principles of management of malnutrition and sarcopenia, including guidance on optimising nutritional intake through diet and the inclusion of oral nutritional supplements when indicated, in combination with exercise.
The fact sheet is available free to healthcare professionals and can be downloaded at: www.malnutritionpathway.co.uk/sarcopenia
Figure 1: Some of the consequences of muscle mass
 References: 1. Deutz NE, et al. (2014). Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr.; 33(6): 929–936. 2. Cruz-Jentoft AJ, Sayer AA (2019). Sarcopenia. Lancet; 393(10191): 2636–2646. 3. Kenny RA, Romero-Ortuno R, Kumar P (2017). Falls in older adults. Medicine; 45(1): 28–33. 4. Bozzetti F (2017). Forcing the vicious circle: sarcopenia increases toxicity, decreases response to chemotherapy and worsens with chemotherapy. Ann Oncol.; 28(9): 2107–2118. 5. Byun MK, et al. (2017). Sarcopenia correlates with systemic inflammation in COPD. Int J Chron Obstruct Pulmon Dis.; 12: 669–675. 6. Springer J, Springer JI, Anker SD (2017). Muscle wasting and sarcopenia in heart failure and beyond: update 2017. ESC Heart Fail.; 4(4): 492–498. 7. Landi F, et al. (2017). The association between sarcopenia and functional outcomes among older patients with hip fracture undergoing in-hospital rehabilitation. Osteoporos Int.; 28(5): 1569–1576.
References: 1. Deutz NE, et al. (2014). Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr.; 33(6): 929–936. 2. Cruz-Jentoft AJ, Sayer AA (2019). Sarcopenia. Lancet; 393(10191): 2636–2646. 3. Kenny RA, Romero-Ortuno R, Kumar P (2017). Falls in older adults. Medicine; 45(1): 28–33. 4. Bozzetti F (2017). Forcing the vicious circle: sarcopenia increases toxicity, decreases response to chemotherapy and worsens with chemotherapy. Ann Oncol.; 28(9): 2107–2118. 5. Byun MK, et al. (2017). Sarcopenia correlates with systemic inflammation in COPD. Int J Chron Obstruct Pulmon Dis.; 12: 669–675. 6. Springer J, Springer JI, Anker SD (2017). Muscle wasting and sarcopenia in heart failure and beyond: update 2017. ESC Heart Fail.; 4(4): 492–498. 7. Landi F, et al. (2017). The association between sarcopenia and functional outcomes among older patients with hip fracture undergoing in-hospital rehabilitation. Osteoporos Int.; 28(5): 1569–1576.
Low awareness of vitamin D could be putting the nation’s bone health at risk
Vitamin D is essential for healthy bones, but few people know how to get enough, according to new research.
Despite vitamin D being essential for healthy bones, only half of people (51%) realise that it is important for bone health and 43% have never even considered what they need to do to look after their bones, according to a recent poll of 2,000 UK adults by YouGov and commissioned by the Royal Osteoporosis Society (ROS)*.
Dr Rosemary Leonard MBE is joining forces with the ROS to raise awareness of this important vitamin, and the need to protect our bones throughout life.
Rosemary said: “The benefits of getting enough vitamin D are huge for bone health because having low levels can increase your risk of osteoporosis and broken bones.
There's a small amount of vitamin D in some foods, but it's difficult to get enough from food alone, so what we absorb via sunlight is vital. Supplements can also be a useful way to top up too.”
Unfortunately, the recent poll showed less than four in ten (37%) people realise that you can only get vitamin D from sunlight between April and September in the UK.
Rosemary said: “From April through the summer we can get good amounts of vitamin D from sunlight. During these months, it's recommended that you expose your skin for short periods to direct sunlight for around 10 minutes, once or twice a day. From the end of September to the beginning of April though, we should all consider taking a daily 10 microgram vitamin D supplement because we can’t get it from sunlight.”
While people may be missing out on vitamin D from the sun at key times of year, recent polling has shown that 49% of people are also missing out on vitamin D during the autumn, and winter, months by not supplementing their intake.
Half of women and 20% of men over 50 years old will break a bone because of osteoporosis1 – a condition where your bones become weak and break more easily – so, it’s never too early or too late to act on your bone health.
You can find out more about vitamin D, nutrition and exercise for good bone health on the Royal Osteoporosis Society website: www.theros.org.uk.
*All figures, unless otherwise stated, are from YouGov Plc. Total sample size was 2,082 adults. Fieldwork was undertaken between 21-22 April, 2021. The survey was carried out online. The figures have been weighted and are representative of all UK adults (aged 18+).1. Van Staa TP, Dennison EM, Leufkens HG, Cooper C. Epidemiology of fractures in England and Wales. Bone. 29(6)517-22 (2001).
To find out more about the Bone Health Accreditation Scheme, you can visit www.ros.org.uk/accreditation
Drinking any type of coffee associated with reduced risk of chronic liver disease
Drinking coffee that is caffeinated or decaffeinated, ground or instant, has been associated with a reduced risk of developing chronic liver disease and related liver conditions, according to a study published in the open access journal BMC Public Health.
Researchers at the Universities of Southampton and Edinburgh, UK, found that drinking any type of coffee was associated with a reduced risk of developing and dying from chronic liver disease compared to not drinking coffee, with the benefit peaking at three to four cups per day.
The authors studied UK Biobank data on 495,585 participants with known coffee consumption, who were followed over a median of 10.7 years to monitor who developed chronic liver disease and related liver conditions.
Of all participants included in the study, 78% (384,818) consumed ground or instant caffeinated or decaffeinated coffee, while 22% (109,767) did not drink any type of coffee. During the study period, there were 3,600 cases of chronic liver disease, including 301 deaths. Additionally, there were 5,439 cases of chronic liver disease or steatosis (a build of up fat in the liver also known as fatty liver disease), and 184 cases of Hepatocellular carcinoma, a type of liver cancer.
Compared to non-coffee drinkers, coffee-drinkers had a 21% reduced risk of chronic liver disease, a 20% reduced risk of chronic or fatty liver disease, and a 49% reduced risk of death from chronic liver disease. The maximum benefit was seen in the group who drank ground coffee, which contains high levels of the ingredients Kahweol and cafestol, which have been shown to be beneficial against chronic liver disease in animals.
Instant coffee, which has low levels of Kahweol and cafestol was also associated with a reduced risk of chronic liver disease. While the reduction in risk was smaller than that associated with ground coffee, the finding may suggest that other ingredients, or potentially a combination of ingredients, may be beneficial.
Dr Oliver Kennedy, the lead author said: "Coffee is widely accessible and the benefits we see from our study may mean it could offer a potential preventative treatment for chronic liver disease. This would be especially valuable in countries with lower incomes and worse access to healthcare and where the burden of chronic liver disease is highest."
Paper: All coffee types decrease the risk of adverse clinical outcomes in chronic liver disease: a UK Biobank study. BMC Public Health: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-10991-7
New funding for research into remote healthcare for eating disorders during the COVID-19 pandemic and beyond
Previous research has revealed concerns around the suitability of current remote healthcare.
Northumbria University health and cyber psychologist Dr Dawn Branley-Bell has been awarded a Medical Research Foundation Fellowship – one of four projects supported by £1.1 million of new funding to tackle eating disorders and self-harm.
A new project led by Research Innovation Fellow Dr Branley-Bell from Northumbria University’s Department of Psychology will explore what we can learn about the causes, prevention and future treatment of eating disorders following the rapid transition to remote care during the COVID-19 pandemic.
Approximately 1.25 million people in the UK have an eating disorder. Recent research by Dr Branley-Bell suggests that many individuals with eating disorders have experienced worsened symptoms during the COVID-19 pandemic and reported concerns around the suitability of healthcare delivered remotely.
Such concerns included, for example, individuals seeing themselves more often on video calls, giving more opportunities to be self-critical of their appearance, or being asked to weigh themselves at home.
Building on her previous research, Dr Branley-Bell will now work alongside people with lived experience of eating disorders, healthcare providers, eating disorder charities, technology designers and other experts in the field to identify why symptoms worsened during the pandemic and to explore the challenges experienced with remote treatment.
The Medical Research Foundation scheme provides postdoctoral researchers the opportunity to start independent, internationally competitive research careers in the field of eating disorders and self-harm. This research project, and the Medical Research Foundation’s previous investments in eating disorders and self-harm research, have been made possible by a gift in Will from Catherine Evans. Help the Medical Research Foundation continue to support much-needed research into eating disorders and self-harm, by joining their team of walkers for the Thames Bridges Trek on 11 September 2021. Find out more on their website. longitudinal prospective cohort study. J Acad Nutr Diet.; doi: 10.1016/j.jand.2021.04.014.
Upgrading staff’s PPE on COVID-19 wards cuts hospital-acquired infections almost completely
Addenbrooke’s Hospital in Cambridge upgraded its face masks for staff working on COVID-19 wards to filtering face piece 3 (FFP3) respirators and saw a dramatic fall – up to 100% – in hospital-acquired SARS-CoV-2 infections among these staff.
The findings are reported by a team at the University of Cambridge and Cambridge University Hospitals (CUH) NHS Foundation Trust. The research is yet to be peer-reviewed, but is being released early because of the urgent need to share information relating to the pandemic.
Until recently, advice from Public Health England recommended that healthcare workers caring for patients with COVID-19 should use fluid resistant surgical masks type IIR (FRSMs) as respiratory protective equipment. If aerosol-generating procedures were being carried out, then the guidance recommended the use of an FFP3 respirator. PHE has recently updated its guidance to oblige NHS organisations to assess what risk transmission of COVID-19 poses to their staff and provide FFP3 respirators where appropriate.
Since the start of the pandemic, CUH has been screening its healthcare workers regularly for SARS-CoV-2, even where they show no symptoms. They found that healthcare workers caring for patients with COVID-19 were at a greater risk of infection than staff on non-COVID-19 wards, even when using the recommended respiratory protective equipment. As a result, its infection control committee implemented a change in respiratory protective equipment for staff on COVID-19 wards, from FRSMs to FFP3 respirators.
Prior to the change in respiratory protective equipment, cases were higher on COVID-19 wards compared with non-COVID-19 wards in seven out of the eight weeks analysed by the team. Following the change in protective equipment, the incidence of infection on the two types of ward was similar.
The results suggest that almost all cases among healthcare workers on non-COVID-19 wards were caused by community-acquired infection, whereas cases among healthcare workers on COVID-19 wards were caused by both community-acquired infection and direct, hospital-based infection from patients with COVID-19 – but that these direct infections were effectively mitigated by the use of FFP3 respirators.
To calculate the risk of infection for healthcare workers working on COVID-19 and non-COVID-19 wards, the researchers developed a simple mathematical model.
Dr Mark Ferris from the University of Cambridge’s Occupational Health Service, one of the study’s authors, said: “Healthcare workers – particularly those working on COVID-19 wards – are much more likely to be exposed to coronavirus, so it’s important we understand the best ways of keeping them safe."
“Based on data collected during the second wave of the SARS-CoV-2 pandemic in the UK, we developed a mathematical model to look at the risks faced by those staff dealing with COVID-19 patients on a day-to-day basis. This showed us the huge effect that using better PPE could have in reducing the risk to healthcare workers.”
According to their model, the risk of direct infection from working on a non-COVID-19 ward was low throughout the study period, and consistently lower than the risk of community-based exposure.
By contrast, the risk of direct infection from working on a COVID-19 ward before the change in respiratory protective equipment was considerably higher than the risk of community-based exposure. CUH staff on COVID-19 wards were at 47 times greater risk of acquiring infection while on the ward than staff working on a non-COVID-19 ward.
Crucially, however, the model showed that the introduction of FFP3 respirators provided up to 100% protection against direct, ward-based COVID-19 infection.
The research was funded by Wellcome, the Addenbrooke’s Charitable Trust, UK Research and Innovations, and the NIHR Cambridge Biomedical Research Centre.
Reference: Ferris, M, Ferris, R et al. FFP3 respirators protect healthcare workers against infection with SARS-CoV-2. DOI: 10.22541/au.162454911.17263721/v1The text in this work is licensed under a Creative Commons Attribution 4.0 International License. Images, including our videos, are Copyright ©University of Cambridge and licensors/contributors as identified. All rights reserved. We make our image and video content available in a number of ways – as here, on our main website under its Terms and conditions, and on a range of channels including social media that permit your use and sharing of our content under their respective Terms.