2019 BAPEN Annual Conference
The highlights

Pete Turner (Chair) & Jennie Mort (Sovereign Conference), BAPEN Programmes Committee, along with the Symposia Chairs Carolyn Wheatley, Jutta Koeglmeier, Mary Phillips, Dr Jeremy Nightingale & Anne Holdoway report on this year’s BAPEN Conference.
This year’s BAPEN Annual Conference, held in Belfast, attracted over 590 attendees. The conference offered delegates an extensive range of clinical and scientific topics relevant to both acute and community settings; providing over 13 symposia, the Pennington and Keynote Lectures, the Nutricia breakfast symposium, 2 satellite symposia sponsored by Abbott and Takeda, and chaired poster sessions incorporating top scoring abstracts. Delegates were exposed to cutting-edge and innovative practice, with the conference providing an abundance of practical take home messages to facilitate improvements in the delivery of nutritional care back in the workplace.
Whilst it is not possible to describe all of the sessions in detail, this review provides insight into some of the conference highlights.
Opening symposium
The opening session in Belfast, Good Morning BAPEN saw the launch of the animation video Nutrition matters, BAPEN matters – it recognises the patient journey and includes those at home, patients placed at the centre of BAPEN. If you’ve not seen it yet, please click here to take a look. This nicely led into BAPEN and the patient journey. As a core group of BAPEN, PINNT supports people on home artificial nutrition (HAN) and are part of this patient journey, and Chair of PINNT Carolyn Wheatley reflected on 2019 and outlined relevant resources they had produced to support their members. These include ‘Living with artificial nutrition’ and, the second booklet in the trilogy, ‘Transition for young people with intestinal failure.’ PINNT believe life on HAN is achievable, often to a good standard, but we need to ensure we encompass every potential outcome, recognising the highs and lows and the effort and achievements of all people on HAN, not just those who make the headlines. To this end, PINNT ran a success HAN week in August, which encouraged people to celebrate ‘This is Me!’. It was an inclusive initiative for those on HAN, healthcare professionals and industry alike, all playing a vital role in the overall delivery and process for homecare. PINNT highlighted the value of partnerships – collectively resources and information can reach more people on HAN and provide credible and valuable assistance for those on HAN.
As both BAPEN and PINNT are committed to improving care for people on HAN support, we committed to a piece of work that was launched in January. All too frequently we hear that home enteral nutrition (HEN) patients feel unheard and under supported, so we will be asking them what they think. The results of this survey will inform a 2020 work stream to ascertain if the NICE Quality Standards – Nutrition Support in Adults (2012) are being adhered to. The goal is to raise awareness amongst people on home enteral tube feeding as to what they can expect from healthcare organisations who are responsible for their nutritional care. HAN Week 2020 takes place 3-9 August (see the PINNT update for more info).
Nutrition support in infants and children
The symposium ‘Nutrition support in infants and children’ was jointly organised by BSPGHAN and BPNG and focused on the management of parenteral nutrition in infants and children from birth to adolescence. The first talk given by Alia Hussain, Senior Clinical Pharmacist at University College London Hospital, focused on the issues around the implementation of standard bags on a neonatal unit in London. The second lecture was given by Venetia Simchowitz, Parenteral Nutrition Consultant at Great Ormond Street Hospital for Children in London. Venetia discussed parenteral nutrition regimes for infants and children in the hospital setting and the implications of the updated ESPGHAN parenteral nutrition (PN) guidelines published in 2018. The third speaker was Professor Andrew Gennery, Consultant in Paediatric Immunology and HSCT at Newcastle University Hospital. Professor Gennery spoke about how to manage the fluid and nutrient requirements of children with complex health needs after a bone marrow transplant. The last part of the symposium was dedicated to the presentation of a new way of checking the correct position of nasogastric feeding tubes in adults. A paediatric study day is planned for the future.
Assessment/early management of a patient with active surgical intestinal failure
BIFA organised two sessions with the NNNG, the first on Assessment/early management of a patient with acute surgical intestinal failure. Marie Sheahan and Dr Nikki Burch both presented cases. On the expert panel were Dr Alison Culkin, Georgie Adams and Aminda De Silva. Both cases induced a large amount of discussion especially on the surgical management. The key message was to wait (months) before definitive surgery is performed to re-establish bowel continuity. During this time, sepsis is treated and a good nutritional status achieved. Experience of largely tropic distal enteral feeding was presented by James Willsmore.
Discharging a patient on HPN
The second joint symposium from BIFA and the NNNG covered Discharging a patient on HPN (home parenteral nutrition) and began with the Nightingale Trust for Nutritional Support Pam Harris Medal Lecture which was awarded to Hayley Leyland on repairing long-term feeding catheters. Then followed a case, presentations and discussions all relating to discharging patients on HPN in England (presented by Mia Small), Wales (presented by Sarah Arnold), Scotland (presented by Gillian Kyle) and Northern Ireland (presented by Emma Murray and Rosie Smith). The symposium concluded with a discussion about the problems that occur when a homecare company suddenly becomes unable to supply PN.
Gastroparesis – diagnosis and treatment options
There were two sessions arranged by BIFA and the local Northern Ireland team (Gerrard Rafferty). The first session covered Gastroparesis – diagnosis and treatment options, which was extremely well reviewed. Dr Asma Fikree talked about the difficulties of making the diagnosis, especially if opiates or cyclizine have been taken. Both these drugs can also make the dysmotility worse. The session also dealt with the interrelationship with psychology by Dr Peter Byrne, and finished with an update about small intestinal transplantation by Dr Lisa Sharkey.
Blood glucose control with parenteral nutrition
The second session entitled Blood glucose control with parenteral nutrition included the current basics of insulin therapy, which were presented by Dr Ailish Nugent; ITU management presented by Professor Greet Van den Berghe; and how to achieve glycaemic control when having PN, presented by Dr Vishakha Bansiya. BIFA will be producing guidance on the management of blood glucose when receiving PN.
COPD – the role nutrition across the continuum of disease
In a symposium dedicated to COPD and the role of nutrition across the continuum of disease, Professor John Hurst from University College London and National COPD Audit Lead, laid the foundations for the symposium by reminding us of the pathophysiology of COPD. With 3 million deaths per year and 33 million DALYs (disability-adjusted life years) lost from this debilitating condition, Professor Hurst illustrated how common and burdensome COPD is and that exacerbation and hospitalisation due to exacerbations, are what matters to patients. Hence exacerbation prevention remains a major goal. Professor Hurst illustrated how phenotypic diversity and multimorbidity warrant bespoke nutritional care. John concluded that if we are to collectively achieve optimal care, COPD clinicians will need the help from experts in nutrition, to not only further understand the impact of nutritional status on disease progression and exacerbations on patients but and determine nutritional interventions that can positively influence outcomes in COPD.
Dr Peter Collins, Lecturer & Research Academic in Nutrition and Dietetics University of Queensland, Australia, followed with a comprehensive review, deftly delivered, on the aetiology of malnutrition in COPD and the evidence supporting oral nutritional interventions in both the community and hospital settings. Peter illustrated the strong case for the use of oral nutritional supplements (ONS) in hospital in-patients to improve energy and protein intakes, which in turn delivered improvements in weight and substantial cost savings through improved outcomes. Against a backdrop of increased inflammation, corticosteroids and immobility, Peter highlighted the challenges in preventing loss of fat free mass during exacerbations and with disease progression. Whilst hospital in-patient stays present an opportune time to diagnose malnutrition and commence nutrition support, Peter emphasised the limitations in reversing malnutrition during a hospital stay, thus emphasising the need for continued, coordinated nutritional care post-discharge. Peter then took us through the data in out-patient settings, reflecting on the significant improvements in nutritional intake, nutritional status and functional capacity, achieved through the use of ready-to-drink oral nutritional supplements (ONS). With data on the use of powdered ONS limited but beginning to emerge – the data has shown adherence to be low (48%) highlighting the need for closer monitoring if powdered ONS are chosen. Provision of food (snacks) is effective and dietary counselling may maximise the effects of ONS. With evidence currently limited in evaluating the effect of nutritional interventions on body composition but consistent improvements in function and quality of life demonstrated through oral nutritional support, Peter encouraged further research to determine the impact of interventions on outcomes that matter to patients.
Natalie Kominek, from Great Western Hospitals NHS Foundation Trust, rounded up the COPD symposium with the results of a pragmatic implementation of the nationally endorsed ‘Managing Malnutrition in COPD in the community pathway’. Through screening and nutritional care according to the ‘Managing Malnutrition in COPD Guide’, the Swindon-based team were able to demonstrate through their pilot study good compliance with ONS over the 12-week intervention period in those at high risk of malnutrition. Approximately half of the patients met their primary nutritional goals (weight maintenance and weight gain) and a significant reduction in overall malnutrition risk was demonstrated. Patient’s self-rating of health and satisfaction with their malnutrition management was high, and cost-savings were achieved through reduced GP visits, reduced prescriptions even when the cost of the dietetic service and products were accounted for.
The nutritional management of pancreatic disease
This symposium covering the nutritional management of pancreatic disease provided an overview of the new NICE guidelines for pancreatitis by Mary Phillips. The primary take home messages were the importance of early enteral feeding and the necessity for aggressive nutritional support in patients with severe disease. Chronic pancreatitis patients need long-term follow up with a systematic nutritional review similar to that offered to patients with coeliac disease, to help manage the long-term complications of malabsorption, diabetes and bone disease. Oonagh Griffin presented her results from her PhD where she ran an intervention study which highlighted the need for a combine approach of nutrition, physical activity, pancreatic enzymes and fish oils in maintaining muscle mass and performance status in this complex patient group. Dr Sinead Duggan gave a very informative overview of type 3c/pancreaticogenic diabetes and the European guidelines recently published on the management of chronic pancreatitis. She explained the pathophysiology of this type of diabetes and the differences in management, predominantly around the co-existence of malabsorption and malnutrition. Finally, an oral presentation was given by Dr Adam McCulloch, University Hospital Birmingham, on the use of PN in patients undergoing cytoreductive surgery with heated intraperitoneal chemotherapy. Dr McCulloch highlighted the complexity of management with this unusual treatment, and the need for accurate nutritional assessment prior to surgery to ensure patients with significant malnutrition receive timely nutrition support.
Against the odds – achieving optimal nutrition support in Upper GI cancer
The symposium ‘Against the odds – achieving optimal nutrition support in Upper GI cancer’ explored the challenges of providing nutritional support following surgery for upper GI cancers. Dr Jessie Elliott, Specialist Registrar in General Surgery, Royal College of Surgeons, Ireland, delivered an expert talk that neatly enhanced our understanding of gut physiology, the role of gut peptides on satiety, appetite, anorexia and the desire to eat, and the emerging knowledge demonstrating that surgery for upper GI malignancies creates similar effects on gut peptides as observed in bariatric surgery, adversely affecting nutritional status in those in whom preservation of weight and nutritional intake need to be optimised to improve outcomes and survival. Building on her own research and knowledge in this field, Jessie outlined the future role and the emerging reality of the use of gut hormones to treat anorexia in the oncology patient. Dr Claire Donohoe, Consultant General and Upper GI surgeon from St James Hospital Cancer Institute/Trinity College Dublin, and Mr Nathan Howes, Consultant General Surgeon, Royal Liverpool and Broadgreen University Hospitals NHS Trust, explored the use of feeding jejunostomy in upper GI cancers – friend or foe? Building on her own research and more widely published literature, Dr Donohoe outlined the journey in her geographical region, to create a framework for nutritional support for patients going through upper GI surgery for cancer. Dr Donohoe outlined the value of jejunosotomy feeding in anastomotic leaks, the presence of other major morbidity and in those failing to thrive but cautioned us on the importance of acknowledging the complication rates and urging us to recognise it is not a panacea. Mr Howes then presented insights into his views on building on the need to apply caution in the use of jejunostomy feeding and reflected on the practice of more selective use of jejunostomy placement. The presentations from the expert panel, along with subsequent interactions with delegates, illustrated the challenges in working towards a consensus. The symposium highlighted that considerable variation in nutrition support practices exist but, in the absence of a ‘crystal ball’ to anticipate those individuals who may run into post-op problems that may further interfere with food intake, there remains a lack of consensus as to the optimal means and duration of nutrition support in patients undergoing surgery for upper GI cancers. The presentations illustrated the many un-answered questions with regards to weight loss and malnutrition after oesophagectomy but did provide a clear overview into our knowledge to date, the conditions and challenges faced by patients in achieving an adequate oral intake, the risks associated with jejunostomy feeds and the benefits of integrating nutrition into prehab and rehab and the pros and cons of selective nutrition support versus feeding all. What was clear was that this field is ripe for further research to optimise outcomes and positively influence the patient experience and how, in the future, we might stratify care and determine nutritional interventions according to predicted risk.
Delivering person-centred care – understanding the patient’s perspective
The symposium on delivering person-centred care focused on understanding the patient’s perspective. Lesley Carter, Clinical Lead for Age UK & Programme Manager at the Malnutrition Task Force, presented on the social and functional needs of older patients and the significant shortfalls in the support they receive, highlighting the most common fears in older patients are cognitive decline and sight loss, therefore these may be most incentivising for behaviour change. This was followed by a fascinating presentation by Dr Kate Reid, a Speech Language Therapist from University Hospital Birmingham, who emphasised the need as healthcare practitioners to adjust our communication styles according to a 5 key patient narrative.

The Pennington Lecture
This year’s prestigious Pennington Lecture ‘Everyman, a journey through clinical nutrition’ was delivered by Dr Alastair McKinlay, Consultant Gastroenterologist, Aberdeen Royal Infirmary. In a highly entertaining lecture, Alastair used an analogy with the sixteenth century religious play ‘Everyman’ to illustrate how the overwhelming good of the multidisciplinary team can overcome ‘evil’ practices in nutritional support. In fact, the presentation was so good, Alastair can almost be forgiven for his quip about dietitians attending catering college!

The John Lennard Jones Keynote Lecture
BAPEN are grateful to Professor Mike Stroud for stepping in at short notice to deliver the inaugural John Lennard Jones Keynote Lecture. Mike’s awe inspiring talk on his polar expeditions and other feats of human endurance not only gave us highly relevant facts on nutrition and body composition but was also highly motivational in demonstrating that with the right frame of mind, human beings of any age and gender can overcome apparently insurmountable physical challenges.
Closing symposium
In the closing symposium, Nutrition Myth Busters, Pete Turner played devil’s advocate to outline three commonly encountered myths in clinical nutrition before a panel of experts attempted to bust the myth and the audience voted ‘myth busted’, ‘myth confirmed’ or ‘myth plausible’.
The first myth was ‘malnutrition causes low albumin and oedema’ and Pete outlined the arguments we all hear frequently in support of it: Low protein intake reduces albumin synthesis and therefore plasma levels. This in turn leads to a decrease in the plasma oncotic pressure that retains fluid within the capillaries and oedema develops – the classic example being kwashiorkor in children.
Professor Mike Stroud set about dispelling this myth with the following points:
- Most malnourished patients, even extreme cases such as anorexia nervosa, do not have low albumin or oedema
- Dietary intakes of oedematous children with kwashiorkor and non-oedematous ones with marasmus are the same including protein intake
- Very low protein intakes do not lead to a drop in albumin synthesis due to amino acids obtained from skeletal muscle and upregulated colonic urea salvage
- Patients with the rare inherited disorder analbuminaemia have an albumin level of 0 g/l but are not oedematous
- ESPEN now categorically state that albumin should not be used as a nutritional marker (Clinical Nutrition 2017; 36: 49-64)
- Nephrotic syndrome, liver disease, SIRS and protein losing enteropathy can all cause low albumin but the main reason for it to occur in our patients is redistribution. Inflammation leads to increased vascular permeability (leaky capillaries) and albumin leaks from the vascular compartment to extravascular compartment
- Oedema is actually caused by increased vascular permeability, salt and water retention in illness, catabolism increasing renal solute load and potassium depletion
- Iatrogenic causes of oedema are common, including high fluid and salt volumes given during sepsis and surgery, IV antibiotics and drugs with a high fluid and sodium content, meaningless fluid balance charts and incompetent IV fluid prescribing
- Oedema usually resolves before albumin levels return to normal.
The audience voted overwhelmingly that the myth was busted and many commented that, although they knew albumin was a poor nutritional marker, such a detailed explanation of the physiology was very welcome.
The second myth was more controversial ‘low carbohydrate diets cause excess weight loss in cancer patients’. Pete explained that although tumours require large amounts of glucose to grow because of the Warburg effect, cutting out carbohydrates and increasing intakes of proteins and fats can cause other metabolic imbalances, enhance cachexia with proinflamatory lipids, feed tumours with amino acids and stop patients taking evidence-based oral nutritional supplements leading to weight loss.
Dietitian Susan Wood rose to the difficult challenge of busting this myth with many valid points including:
- Ketogenic diets are not high in protein
- Ketogenic diets have been shown to have beneficial effects on body composition and cardiovascular health
- Ketogenic diets have been shown to improve body composition in endometrial and ovarian cancer and may slow tumour growth
- Ketones may protect cells from harmful effects of radio and chemotherapy
- Providing overall dietary energy intake is not excessive, there is no evidence fats are harmful.
This was a very difficult subject to tackle and although the audience were split, with most voting myth plausible or myth busted, Susan did a great job as only a few voted myth confirmed. More importantly though, Susan made us really think about a subject that many of us had dismissed without even looking at the evidence.
For the final myth ‘enteral nutrition should be avoided in noninvasive ventilation (NIV)’ Pete explained that NG tubes break the seal of the tight fitting masks, nasal specs and hoods required. Furthermore, because of the high flow air and oxygen, the stomach becomes distended and enteral feeding leads to abdominal discomfort, vomiting, reflux and aspiration.
Dietitian Peter Collins made the flowing points to dispel the myth:
- Equipment is available to stop mask seals being broken with NG tubes
- Studies have shown that enteral feeding is associated with improved outcomes in NIV
- There are published protocols that allow effective feeding in NIV
- The input of an expert dietitian is required.
The symposium experts Mike Stroud, Susan Wood and Peter Collins provided the audience with an entertaining and thought-provoking finale to a fabulous conference.
Other features
A select few were fortunate enough to attend the popular Publication workshop led by Professor Mark Beattie, the new Editor-in-Chief of Frontline Gastroenterology. Again, Professor Beattie provided insight into the world of clinical publishing, with excellent tips, tricks and suggestions to increase the chances of successful publication. Articles on clinical nutrition remain under-represented in comparison to other GI specialities; however, there is a commitment to change this with journals such as Frontline Gastroenterology.
The Exhibition showcased over 30 healthcare companies and not-4-profit organisations with an interest in nutrition, along with BAPEN and the Core Groups – BPNG, BSPGHAN, NNNG, PENG and PINNT.
This year saw the addition of the Nutrition Village, kindly supported by Avanos and BD, where a series of hands on practical sessions were delivered by BAPEN experts in the exhibition area.
This year’s Poster Exhibition displaying over 96 posters, were all presented as oral communications over the two days.
Delegates were invited to attend a Civic Reception at City Hall by kind generosity of Belfast City Council and welcomed to Belfast by Gerry Lennon, Chief Executive, Visit Belfast, which followed with a demonstration from members of the Doherty Petri School of Irish Dancing. This was followed by the BAPEN social event which took delegates to the Belfast Cathedral Quarter to experience the Belfast Craic!
Awards and Recognitions

Presented by Dr Trevor Smith, President, BAPEN
BAPEN ROLL OF HONOUR
Dr Nikki Burch was awarded a Roll of Honour for outstanding contribution to BAPEN as past BAPEN Treasurer, Executive Committee member and BAPEN Medical committee member.

Kate Hall received a Roll of Honour for her contribution to Malnutrition Awareness Week.

BAPEN’s BEST ORAL AND BEST POSTER AWARDS
An Oral Communication Award was presented to Sarah Andersen, Royal Brisbane and Women’s Hospital, for her presentation entitled ‘Nutrition Support and the gastrointestinal microbiome, a systematic review and pilot study’.
The newly named the Professor RG Clark Poster Prize was presented to lead author James Willsmore, Lennard-Jones Intestinal Rehabilitation Unit, St Mark’s Hospital, for his poster entitled ‘Endovascular interventions for the treatment of catheter-related venous thrombosis in patients on home parenteral nutrition’.

POWELL-TUCK PRIZE
BAPEN Medical awarded the Powell-Tuck Prize for the best abstract submitted by a doctor in training also to, James Willsmore.
Congratulations to all our 2020 Award Winners!


BAPEN wish to thank and acknowledge the support received from Visit Belfast and Tourism Northern Ireland

ADVANCE NOTICE
2020 ANNUAL CONFERENCE – 17th & 18th NOVEMBER HILTON BRIGHTON METROPOLE

Facts about BAPEN’s social media campaign during this year’s conference.
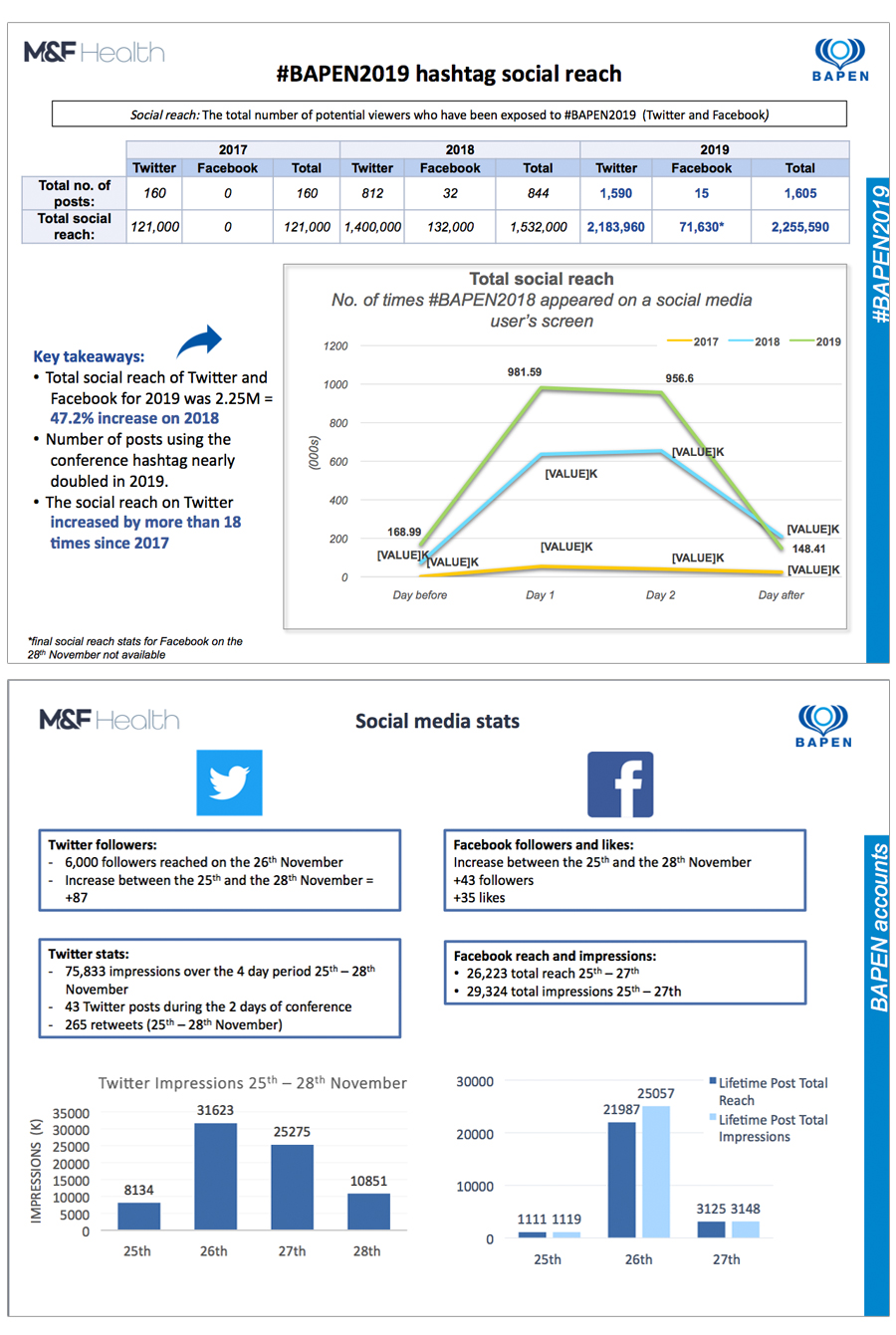
In addition, ICC Belfast provided digital marketing support to BAPEN for this conference and report that overall the google display network was their greatest performing platform, it generated over 1.9m impressions and over 7.2k people to the conference landing page. This achieved a 0.37% click through rate which trumps industry standard of 0.14%. Their Facebook campaign gained over 381k impressions and over 3k clicks.
Year on year they increased pageviews on the conference page by 91%, increased online registrations by 18% year on year and overall generated a 24% increase in overall delegate numbers.
